Pregnancy
LUTEAL PHASE, WHAT IT IS? AND HOW IS RELATED TO PREGNANCY

Last Updated on August 27, 2024 by Joshua Isibor
What Is the Luteal Phase?
The period between ovulation and the beginning of the next menstrual cycle is called the luteal phase. The follicle gets converted to a corpus luteum during this phase. A corpus
luteum is a cell structure that produces high amounts of progesterone and some estrogen. These luteal phase hormones play an important role in pregnancy. This article is about the luteal phase and its relation to pregnancy.
🌟 Luteal phase versus menstrual cycle
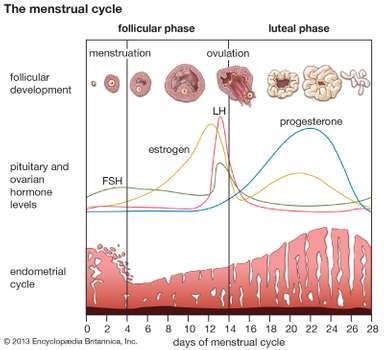
The basics of a woman’s menstrual cycle can be broken down into three sections: the follicular phase, ovulation, and the luteal phase.
The follicular phase begins on the first day of your period and lasts until the ovaries release an egg. When the egg is released, the body enters ovulation, which typically lasts a couple of days before the luteal phase begins.
Finally, the luteal phase is the second half of your cycle. This is when fertilization and implantation can happen. This part of the menstrual cycle lasts between 10 to 16 days,
depending on the woman. At the end of the luteal phase, one of two things will happen: you will either start your period, or you will discover you are pregnant.
The average menstrual cycle lasts about 28 days. Many people think of their cycle as just two parts: the five or six days we bleed and the rest of the month when we don’t. Knowing when your luteal phase occurs is important for those wanting to learn more about their body.
The menstrual cycle has four distinct phases. Being aware of each phase and what is or isn’t normal in each phase is vital to understanding reproductive health.
Some people want to understand their cycle better for trying to conceive, trying to avoid pregnancy, or just trying to figure out why they aren’t feeling well.
The more you understand your menstrual cycle, the sooner you might be able to conceive if desired or notice reproductive health concerns. Understanding each phase, including the luteal phase, is a great way to be an active participant in your healthcare.
🌟 The menstrual cycle.
The menstrual cycle consists of three phases: ovulatory, luteal, and follicular. Each phase is important in fertilizing the ovum and making you pregnant.
If you aren’t pregnant, it also sheds the unused endometrial lining at the termination of the cycle. If you have a normal menstrual cycle of about 25 to 28 days, the luteal phase will last for about 12 to 14 days. If you have a menstrual cycle of less than 25 days, the luteal phase can be shorter.
🌟 Luteal phase
The luteal phase is the latter phase of the menstrual cycle (in humans and a few other animals) or the earlier phase of the oestrous cycle (in other placental mammals). It begins
with the formation of the corpus luteum and ends in either pregnancy or luteolysis. The main hormone associated with this stage is progesterone, which is significantly higher during the luteal phase than in other phases of the cycle. Another is the endocannabinoid,
anandamide AEA, where the lowest plasma AEA level is observed in the luteal phase. The opposite of the luteal phase, the rest of the two weeks, is called the follicular phase.
🌟 Menstrual cycle Hormonal events
After ovulation, the pituitary hormones FSH and LH, released from the anterior pituitary, cause the remaining parts of the dominant follicle to transform into the corpus luteum. It continues to grow for some time after ovulation and produces significant amounts
of hormones, particularly progesterone and to a lesser extent, estrogen.
Progesterone plays a vital role in making the endometrium receptive to blastocyst implantation and supportive of early pregnancy; it also raises the woman’s basal body temperature.
The increased progesterone and BBT will cause at least a modest rise in BMR at the start of the luteal phase, which will remain elevated until the phase ends. However, research has discrepant findings on how much of an increase typically occurs and how much it can vary.
Early, small sample studies have found various figures, such as; a 6% higher postovulatory sleep metabolism, a 7% to 15% higher 24-hour expenditure following ovulation, and an increase and a luteal phase BMR by up to 12%.
A study by the American Society of Clinical Nutrition found that an experimental group of female volunteers had an 11.5% average increase in 24-hour energy expenditure in the two weeks following ovulation, with a range of 8% to 16%. This group was measured via simultaneously direct and indirect calorimetry and had a standardized daily meal and sedentary schedules in order to prevent the increase from being manipulated by a change in food intake or activity level.
A 2011 study conducted by the Mandya Institute of Medical Sciences found that BMR does not significantly differ between a woman’s follicular phase and menstrual cycle. However, the calories burned per hour are significantly higher, up to 18%, during the luteal phase. Increased state anxiety (stress level) also temporarily increases BMR.
Several days after ovulation, the increasing amount of estrogen produced by the corpus luteum may cause one or two days of fertile cervical mucus, lower basal body temperatures, or both. This is known as a “secondary estrogen surge”.
The hormones produced by the corpus luteum also suppress the production of the FSH and LH, which the corpus luteum needs to maintain itself. With continued low levels of FSH and LH, the corpus luteum will atrophy.
The death of the corpus luteum results in falling levels of progesterone and estrogen. These falling levels of ovarian hormones cause increased levels of FSH, which begins recruiting follicles for the next cycle. Continued drops in levels of estrogen and progesterone trigger the end of the luteal phase, menstruation, and the beginning of the next cycle.
The loss of the corpus luteum can be prevented by the implantation of an embryo: after implantation, human embryos produce human chorionic gonadotropin (hCG), which is structurally similar to LH and can preserve the corpus luteum. Because the hormone is unique to the embryo, most pregnancy tests look for the presence of hCG. If implantation occurs, the corpus luteum will continue to produce progesterone (and maintain high basal body temperatures) for eight to twelve weeks, after which the placenta takes over this function.
🌟 HOW LONG DOES THE LUTEAL PHASE LAST?
The human luteal phase lasts between ten and sixteen days, with an average of fourteen days. Luteal phases of less than twelve days may make it more difficult to achieve pregnancy. While luteal phase length varies significantly from woman to woman, it will be fairly consistent for the same woman from cycle to cycle.
🌟 Menstrual cycle chart and luteal phase.
For those trying to conceive, understanding ovulation and the luteal phase (which make up the second half of the cycle) is usually their focus. This chart provides an easy breakdown of each phase of the menstrual cycle.
Menstrual Cycle Chart and luteal phase
Can you get pregnant during the luteal phase? Yes, you can. Since the luteal phase is after ovulation, you have a very real chance of getting pregnant.
🌟 Why Is the Luteal Phase Important for Pregnancy?
The luteal phase is the period between ovulation and menstruation. Therefore, the health and length of the luteal phase will affect fertility.
1. Impact of the Luteal Phase’s Length On Pregnancy
If your period of the luteal phase is less than ten days, then you may find it difficult to become pregnant. The reason behind this is that if your corpus luteum weakens and dies in 9 days, ceasing the luteal phase hormone production, then your uterus starts shredding its lining instantaneously, leaving no time for the fertilized ovum to move from the Fallopian tube to the ovary, and get implanted to the uterus lining.
If your luteal phase is short, you will not get pregnant even if the ovum gets fertilized, because you will get your period before the embryo can stick to the uterus lining.
2. Impact of the Luteal Phase’s Health On Pregnancy
Sometimes, even if the duration of the luteal phase is normal, your body may produce less progesterone during this phase, which can be a problem. A sufficient quantity of progesterone is needed to ensure the healthy thickness of the uterus lining. A low amount of progesterone results in a lining that is not healthy enough to sustain a pregnancy.
Therefore, it is important to have a luteal phase that is of normal length and is healthy as well.
🌟 How to Calculate the Luteal Phase of a Menstrual Cycle
🌟 Also Here are some ways to calculate the length of your luteal phase:
A hormone-specific blood test can determine the accurate length of your luteal phase. You can track your menstrual cycle for approximately 6 months, and observe the patterns of your phases of the menstrual cycle, to calculate an approximate length of the
luteal phase.
✔️ Basal Body Temperature (BBT) Charting:
The BBT of your body increases during ovulation and stays high until the onset of your
upcoming period. Track the temperature from the start of the menstrual cycle, and observe the rise in BBT. The rise in body temperature is a solid confirmation that you are ovulating.
🌟 Formula to Calculate Ovulation Time During Luteal Phase
Day of ovulation = length of the menstrual cycle – length of luteal phase
Assume that for a menstruation cycle that lasts for 29 days, the luteal phase lasts up to 15 days. Assigning these values in the formula:
Day of ovulation = 29
29 (length of the menstrual cycle) – 15 (length of luteal phase)
Day of ovulation = 14
It implies that the 14th day of the menstrual cycle is the day your ovulation occurs.
A prediction kit or calculator for ovulation can also be used to determine the day of ovulation and, hence, the luteal phase.
⭐ Symptoms of the Luteal phase.
1. Light cramping.
2. Spotting/implantation bleeding.
3. Changes in vaginal discharge.
4. Nausea and other digestive changes.
5. Increased sense of smell.
6. Sore breasts.
7. Fatigue.
8. Mood swings and changes.
They may also experience a variety of other signs, similar to PMS. Some women wonder about symptoms as early as 3 days post-ovulation. Generally, however, you’ll simply have to wait and see whether your luteal phase ends with a positive pregnancy test or a new cycle.
⭐Types of the luteal phase.
1. Short luteal phase.
A short luteal phase lasts 8 days or less. The hormone progesterone is essential
for implantation and A successful pregnancy. Because of this, a short luteal phase may contribute to infertility.
When a short luteal phase occurs, the body doesn’t secrete enough progesterone, so the uterine lining doesn’t properly develop. This makes it difficult for a fertilized egg to implant in the uterus.
If you do become pregnant after ovulation, a short luteal phase may result in an early miscarriage.
To sustain a healthy pregnancy, the uterine lining must be thick enough for an embryo to attach itself and develop into a baby.
A short luteal phase can also be caused by the failure of the corpus luteum. If the corpus luteum doesn’t secrete enough progesterone, your uterine lining may shed before a fertilized egg implants, which can cause an earlier menstrual cycle.
⭐What causes a short luteal phase?
A short luteal phase lasts 8 days or less. The hormone progesterone is essential to implantation and successful pregnancy. Because of this, a short luteal phase may contribute to infertility.
When a short luteal phase occurs, the body doesn’t secrete enough progesterone, so the uterine lining doesn’t properly develop. This makes it difficult for a fertilized egg to implant in the uterus.
If you do become pregnant after ovulation, a short luteal phase may result in an
early miscarriage. To sustain a healthy pregnancy, the uterine lining must be thick enough for an embryo to attach itself and develop into a baby.
A short luteal phase can also be due to the failure of the corpus luteum. If the corpus luteum doesn’t secrete enough progesterone, your uterine lining may shed before a fertilized egg implants. This can cause an earlier menstrual cycle.
⭐Symptoms of a short luteal phase
If you have a short luteal phase, you may not
realize there’s a problem. You might not suspect fertility issues until you’re unable to conceive.
If you’re having difficulty getting pregnant, your doctor can investigate further to see if you have LPD.
Symptoms may include:
1. Earlier than normal menstrual cycles
2. Spotting in between periods
3 Inability to get pregnant
4. Miscarriage
⭐Diagnosing short luteal phase.
If you can’t get pregnant, figuring out the underlying cause is the first step to improving your odds of conception. Talk to your doctor about infertility.
They can conduct a variety of tests to determine whether infertility is caused by a short luteal phase or another condition.
You’ll likely have blood tests to check your levels of the following hormones:
1. Follicle-stimulating hormone (FSH), a hormone released by the pituitary gland that regulates ovary function.
2. Luteinizing hormone:] The hormone that triggers ovulation
3. Progesterone, the hormone that stimulates the growth of the uterine lining.
In addition, your doctor may recommend an endometrial biopsy. During the biopsy,
a small sample of your uterine lining is collected and examined under a microscope.
Your doctor can check the thickness of the lining.
They may also order a pelvic ultrasound, to examine the thickness of your uterine lining.
A pelvic ultrasound is an imaging test that uses sound waves to generate pictures
of organs in your pelvic area, including your:
1. Ovaries
2. Uterus
3. Cervix
4. Fallopian tubes
⭐Treatment for short luteal phase
Once your doctor identifies the underlying cause of your LPD, pregnancy may be possible.
In many cases, treating the cause is key to improving fertility.
For example, if a short luteal phase results from extreme exercise or stress, decreasing your activity level and learning stress management can cause the return of a normal luteal phase.
⭐Techniques to improve stress levels include:
1. Decreasing personal obligations
2. Deep breathing exercises
3. Meditation
4. Moderate exercise
Your doctor may also recommend supplemental human chorionic gonadotropin (hCG), which is a pregnancy hormone. Taking this supplement can help your body secrete a higher level of the hormone progesterone.
Your doctor may also recommend taking additional progesterone supplements after ovulation. This helps your uterine lining grow to a point where it can support the implantation of a fertilized egg.
Other methods to increase your chance of getting pregnant include; medications, such as clomiphene citrate, which stimulates your ovaries to produce more follicles and release more eggs.
Not all treatments work for every woman, so you’ll have to work closely with your doctor, to find the most effective medication or supplement.
⭐Long Luteal Phase or Pregnant?
Long luteal phase?… Am I pregnant?… It’s probably a safe bet that most women who are ready to start a family have a basic knowledge of their menstrual cycle. You might know
that you have a period, for instance, and you probably also know that you ovulate. You might also be aware that the average woman’s cycle is around 28 days long. But what
about the more minute details of a woman’s reproductive cycle? Would you be able to tell if your period was late, or if you were pregnant? Identifying one or the other of the options is important to a hopeful couple.
Long menstrual cycles can be a frustrating source of false hope – so knowing how to recognize the signs of a long luteal cycle versus a pregnancy can relieve some of the stress a couple may feel as they try to conceive.
⭐ Signs of a long luteal phase or pregnancy.
So how do you know the difference between a successful conception and a long luteal phase? What are the signs? Here are a few indicators that can help you identify which
the stage you’re at before taking a test:
1. Know when to look.
Before you begin to detect a pregnancy naturally, you’ll want to track your full cycle for a couple of months. To do this, you can monitor when your periods start and end and even incorporate ovulation tracking methods. This way, you’ll be fully aware of when each phase will typically begin—and you’ll know when to look for the subtle signs of early pregnancy.
2. Look for implantation bleeding.
Sure, when you’re waiting for your period to show up and you notice spotting, it’s easy to assume that you’re not pregnant. You could, however, be experiencing implantation bleeding, which is a very early sign of pregnancy. Pay attention to what happens next. If you don’t get your full period, then it could be a sign of conception.
3. Watch out for tender breasts.
Sore breasts are a well-known sign of pregnancy. They occur because hormones flood the body once the egg is fertilized, which increases the volume of blood. This adds to the heaviness of the breasts and can make them feel “overfilled.”
However, tender breasts are also a sign of PMS so pay attention to your usual premenstrual signs before trying to get pregnant so you’ll be able to spot the difference in sensations.
4. Notice the loss of energy.
If you’re feeling exhausted and like you just can’t catch up on sleep no matter what you do, it might be a sign of early pregnancy. Women in their first trimesters often experience a complete lack of energy because of the body’s hormone fluctuations and increased blood production. However, many factors add to feeling tired – including;
anxiety, lack of sleep, and even the stress of infertility for those who have been trying to get pregnant for some time. Be sure to maintain a healthy lifestyle while you’re conceiving so you’ll be able to detect these small changes.
The easiest way to determine pregnancy is by taking a simple at-home test. But for women who are trying to get pregnant, knowing and paying attention to their bodies is one of the best things they can do during this time—that way, they won’t be frustrated if they experience an extended luteal phase. They’ll be able to assess their bodies during the conception process and understand their various changes.
⭐ Body Changes in Luteal Phase
Changes in hormonal levels during the luteal phase.
During the luteal phase, the upsurge in progesterone levels
can result in the following body changes:
1. Mood swings
2. Tiredness
3. Tender nipples and breasts
4. Bloating
5. Anxiety
6. Fluid retention
These changes are bound to happen and do not lower your likelihood of getting pregnant.
⭐How Can You Test Your Progesterone Level?
Progesterone levels in the luteal phase are generally higher than in other phases of the menstrual cycle. Your progesterone levels should be tested when they are highest, i.e., on the 21st day of a normal 28-day menstrual cycle, in the middle of the luteal phase.
Of course, it is not given that all women have a typical 28-day menstrual cycle. If you have a 34-day menstrual cycle, with ovulation occurring around the 22nd day, then you cannot
test your progesterone level on day 21, as the results might show a very low level of the hormone. But, if you test it on the 28th day, your progesterone level may be normal.
Hence, if you want to know when you ovulate and the length of your luteal phase, tell your doctor when the right time to test your progesterone levels is.
⭐ How Can You Increase the Luteal Phase?
Taking the following supplements might help to lengthen your luteal phase:
1. Vitamin C – it increases fertility in some cases where women have short luteal phases.
2. Progesterone supplementation or cream – Progesterone can increase your progesterone levels, but please consult your doctor before using this.
⭐ What is a Luteal Phase Defect?
Luteal phase defect or luteal insufficiency is the deficient release of progesterone all through the luteal phase. The insufficiency of progesterone will not thicken the uterus lining, which can result in improper embryo plantation. Hence, it reduces
the chances of a pregnancy continuing. However, it is not yet confirmed if a luteal phase defect is a reason for infertility.
A luteal phase defect can lead to the following problems:
1. Improper working of corpus luteum, which results in lesser production of estradiol and progesterone.
2. Incapability of the uterus lining to react to normal levels of estradiol and progesterone.
⭐ Causes of luteal phase defects.
LPD can be caused by certain conditions, such as:
1. Endometriosis is a condition in which tissue normally found inside the uterus starts to grow outside the uterus.
2. Polycystic ovarian syndrome (PCOS), a disorder that causes enlarged ovaries with small cysts thyroid disorders, such as an overactive or an underactive thyroid, Hashimoto’s thyroiditis, and iodine deficiency.
3. Obesity
4. Anorexia
5. Excessive exercise
6. Aging
7. Stress
A luteal phase defect could also happen due to the following reasons:
1. Defect in the egg.
2. Breakdown of corpus luteum.
3 Un-ruptured follicle.
4. Thyroid disorders
5. Over-exercise
6. Anorexia
7. Endometriosis
8. Polycystic ovary syndrome
9. Obesity
10. Hyperprolactinemia
⭐ Symptoms of Luteal Phase Defect
The symptoms of a luteal phase defect are as follows:
1. Miscarriages.
2. Spotting in between periods.
4. Menstrual cycles are way earlier than normal.
⭐Diagnosis of a Luteal Phase Defect.
A luteal phase defect can be diagnosed by
getting the following tests done:
1. Blood tests
These tests check the level of:
✔️ Progesterone, which helps in the thickening of the uterus lining.
✔️ Follicle-stimulating hormone, which regulates ovarian functions.
✔️ Luteinizing hormone, which triggers ovulation.
✔️ Ultrasound; It helps to find the thickness of the uterus lining. An ultrasound scan
can help detect the functioning of the reproductive organs, i.e. the uterus, ovaries, cervix, and Fallopian tubes.
⭐Treatment Options for Luteal Phase Defect. The treatment of a luteal phase defect depends on the main underlying causes.
1. Human Chorionic Gonadotropin: It releases progesterone and triggers ovulation. During this process, the hCG level is given in a single dosage of 10,000 IU or two dosages of 5,000 IU, given once in 2 weeks to extend the luteal phase.
2. Clomiphene Citrate: These are also called human menopausal gonadotropins. They help stimulate the ovaries to produce more follicles, which release more eggs.
3. Suppositories: Crinone, a vaginal gel, is used vaginally three times a day. The gel holds a progesterone dosage of 90 mg.
4. Pill Treatment: Prometrium oral progesterone medicines are administered at a 200 mg dosage per day.
5. Injections: Intramuscular progesterone is administered at a dose of 25 to 50 mg per day. The injection uses crystalline, odourless progesterone powder dissolved in sesame oil.
The luteal phase, which lasts around 14 days, is the time when the female body prepares the womb for the fertilized ovum. You should have a luteal phase of both sufficient length and health to sustain a pregnancy. You can consult a doctor for mid-luteal phase progesterone
test to check if everything is normal.
ALSO, READ Is pregnancy possible after vasectomy?
Originally posted 2020-11-21 11:26:22.


-


 Text Messages8 months ago
Text Messages8 months agoBEST LOVE CONFESSION MESSAGES FOR HER OR HIM
-



 Sex Education1 day ago
Sex Education1 day ago10 Simple Hack to Make a Girl Send Her Nudes
-


 Text Messages8 months ago
Text Messages8 months agoHeart Touching RIP Uncle Quotes
-



 Health2 months ago
Health2 months ago5 Unknown Ways To Maintain Skin Health
-



 Text Messages8 months ago
Text Messages8 months agoBest Good Luck Wishes Before and After Surgery, for Family and Friends
-


 Text Messages8 months ago
Text Messages8 months agoFreaky and Dirty Paragraphs For Him Copy And Paste Yahoo
-



 Uncategorized6 days ago
Uncategorized6 days agoHOW TO FALL IN LOVE WITH YOURSELF
-



 Uncategorized1 month ago
Uncategorized1 month agoHOW TO KISS A BOY FOR THE FIRST TIME